Abstract
Introduction Autoimmune hemolytic anemia (AIHA) is a clinically heterogeneous collection of disorders characterized by the presence of autoantibodies against the patient's erythrocytes. AHIA has been associated with an increased risk of thromboembolic events, including stroke. A recent nationwide cohort study from Denmark and France showed an increased risk of ischemic stroke compared to the general population. However, no extensive studies have been done in the United States (US); hence, we conducted a study of stroke and AIHA in the US population.
Methods This is a retrospective study from 1999 to 2022. We analyzed data from a nationwide commercial database (Explorys, IBM) that aggregates records from 26 healthcare systems spread over 50 states with almost 80 million patients. It is a cloud-based platform in which participating institutions provide de-identified data from electronic health records. Pooled data is then standardized and normalized. Explorys uses Systemized Nomenclature of Medicine - Clinical Terms (SNOMED CT) coding for medical diagnosis. We identified adult patients (over 18 years old) with the diagnosis of AIHA. Patients with stroke were identified with the following SNOMED-CT diagnosis "cerebrovascular accidents''. In addition, we obtained information on risk factors for stroke, including sex, age over 65 years, and comorbidities known to be a risk factor, including hypertension, atrial fibrillation, diabetes mellitus, hyperlipidemia, smoking, and obesity.Multivariable logistic regression adjusting for all covariates was created to test for stroke. Results were presented as odds ratio (OR) with a corresponding 95% confidence interval (CI). All tests were two-sided, and a p-value ≤ 0.01 was considered statistically significant.
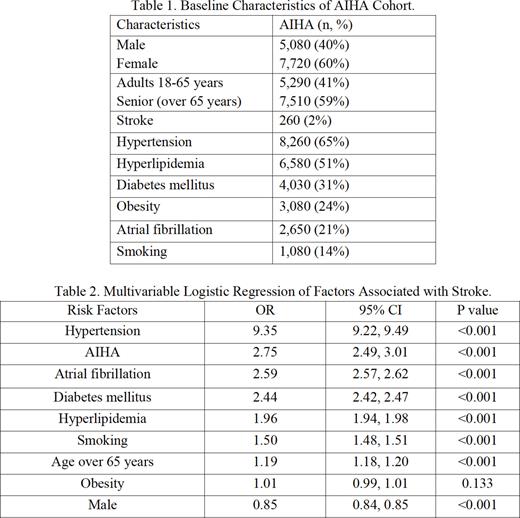
Results An adult population of 69,339,860 were included. AHIA was diagnosed in 12,800 patients (less than 1 per 100,000) and stroke was diagnosed in 238,860 (0.34%). AIHA population characteristics were; females 7,720 (60%), age over 65 years 7,510 (59%), stroke 260 (2%), hypertension 8,260 (65%), hyperlipidemia 6,580 (51%), diabetes mellitus 4,030 (31%), obesity 3,080 (24%), atrial fibrillation 2,650 (21%), and smoking 1,080 (14%). Baseline characteristics are shown in table 1. Statically significant OR of covariates tested is as follows; hypertension OR 9.35 (95% CI 9.22-9.49), AHIA OR 2.75 (95% CI 2.49 - 3.01), atrial fibrillation OR 2.59 (95% CI 2.57 - 2.62), diabetes mellitus 2.44 (95% CI 2.42, 2.47), hyperlipidemia OR 1.96 (95% CI 1.94, 1.98), smoking OR 1.5 (95% CI 1.94, 1.98), age over 65 years OR 1.19 (95% CI 1.18, 1.20), and male OR 0.85 (95% CI 0.84, 0.85). Multivariable logistic regression of factors associated with stroke is shown in table 2.
Discussion and conclusion This is the largest population-based study analyzing the association between AIHA and stroke, and we included the most relevant confounding risk factors in our analysis. As expected, the strongest risk factor associated with stroke was hypertension. What was surprising was that AIHA followed it as the second strongest risk factor, which exceeded atrial fibrillation as a risk factor. Limitations of the retrospective design of the study are numerous. They include lack of patient-level data, the subtype of stroke, the subtype of AIHA, the severity of AIHA, temporality, medications used, and their implications on stroke risk, and inaccuracies in coding. A potential explanation for increased thrombosis includes depletion of nitric oxide as a consequence of intravascular hemolysis with resultant enhanced platelet adhesions, and another possible mechanism is the release of procoagulant microparticles during hemolysis. While there is an ongoing trial looking into long-term apixaban in the primary prevention of venous thromboembolism in AIHA (NCT05089227), no active study is looking into minimizing stroke risk. Prospective studies to affirm association, risk stratifies patients, and ultimately test the utility of prophylactic anticoagulation are most needed.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal